World Well being Group. WHO Tips for Malaria, 3 June 2022. Report No. WHO/UCN/GMP/2022.01 Rev.2 (World Well being Group, 2022).
Esu, E. B., Oringanje, C. & Meremikwu, M. M. Intermittent preventive remedy for malaria in infants. Cochrane Database Syst. Rev. 7 (Cd011525). https://doi.org/10.1002/14651858.CD011525.pub3 (2021).
Ross, A., Maire, N., Sicuri, E., Smith, T. & Conteh, L. Determinants of the cost-effectiveness of intermittent preventive remedy for malaria in infants and kids. PLOS ONE. 6, e18391. https://doi.org/10.1371/journal.pone.0018391 (2011).
Ross, A. et al. Modelling the epidemiological impression of intermittent preventive remedy towards malaria in infants. PLOS ONE. 3, e2661. https://doi.org/10.1371/journal.pone.0002661 (2008).
World Well being Group. WHO Technical Session To Assessment the Function of Medication in Malaria Prevention for Individuals Residing in Endemic Settings (Malaria Coverage Advisory Committee Assembly, 2019). Report No. WHO/UHC/GMP/MPAC/2020.03.
World Well being Group. World malaria report 2009. (Geneva: World Well being Group. (2009). https://www.who.int/publications/i/merchandise/9789241563901.
Benn, C. S. & Aaby, P. Does IPTi lower malaria morbidity however not mortality? Lancet 380, 958–960. https://doi.org/10.1016/S0140-6736(12)61184-2 (2012).
Schellenberg, D., Cisse, B. & Menendez, C. The IPTi consortium: analysis for coverage and motion. Traits Parasitol. 22, 296–300. https://doi.org/10.1016/j.pt.2006.05.006 (2006). https://doi.org/https://doi.org/
Unitaid & Perennial Malaria Chemoprevention (PMC). : The Unitaid IPTi + Mission addressing the hole between WHO steering and nation implementation. (RBM MiP Annual Assembly: Accra, Ghana. (2022). https://endmalaria.org/websites/default/recordsdata/3bpercent20J.Kouakou_IPTipercent2Bpercent20Project.pdf.
Unitaid. The plus undertaking lowering morbidity and mortality attributable to malaria and anemia in youngsters underneath 2. (2023). https://www.psi.org/undertaking/plusproject/.
World Well being Organisation. WHO Tips for Malaria, 16 October 2023. Report No. WHO/UCN/GMP/2023.01 Rev.1 (World Well being Group, 2023).
Kobbe, R. et al. A randomized managed trial of prolonged intermittent preventive antimalarial remedy in infants. Clin. Infect. Dis. 45, 16–25. https://doi.org/10.1086/518575 (2007).
Mockenhaupt, F. P. et al. Intermittent preventive remedy in infants as a method of malaria management: a randomized, double-blind, placebo-controlled trial in Northern Ghana. Antimicrob. Brokers Chemother. 51, 3273–3281. https://doi.org/10.1128/aac.00513-07 (2007).
Grobusch, M. P. et al. Intermittent preventive remedy towards malaria in infants in Gabon–a randomized, double-blind, placebo-controlled trial. J. Infect. Dis. 196, 1595–1602. https://doi.org/10.1086/522160 (2007).
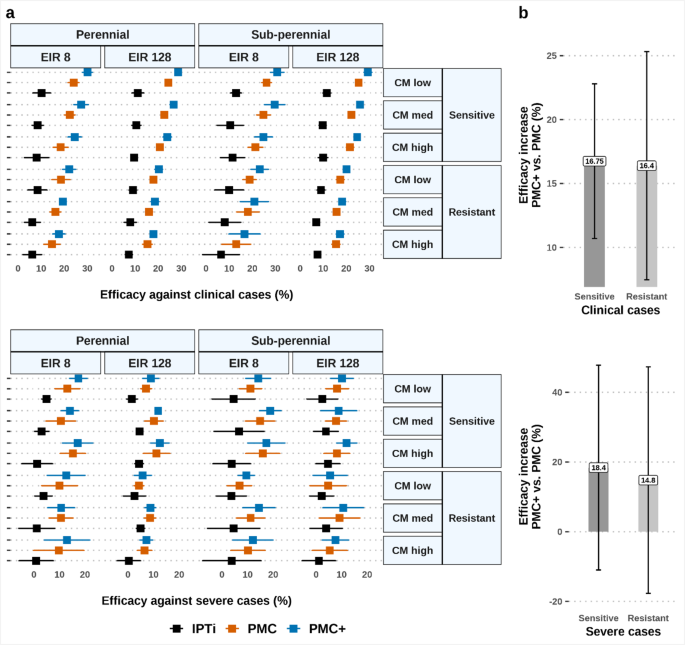
Runge, M. et al. Perennial malaria chemoprevention with and with out malaria vaccination to scale back malaria burden in younger youngsters: a modelling evaluation. Malar. J. 22, 133. https://doi.org/10.1186/s12936-023-04564-9 (2023).
Bigira, V. et al. Protecting efficacy and security of three antimalarial regimens for the prevention of malaria in younger Ugandan youngsters: a randomized managed trial. PLoS Med. 11, e1001689. https://doi.org/10.1371/journal.pmed.1001689 (2014).
World Well being Group. Technical session on the malaria rebound phenomenon: report on a digital assembly, 22–23 March 2022. (Geneva: World Well being Group. (2022). https://apps.who.int/iris/deal with/10665/361710.
Greenwood, B. et al. Resurgent and delayed malaria. Malar. J. 21, 77. https://doi.org/10.1186/s12936-022-04098-6 (2022).
Schellenberg, D. et al. Intermittent preventive antimalarial remedy for Tanzanian infants: follow-up to age 2 years of a randomised, placebo-controlled trial. Lancet 365, 1481–1483. https://doi.org/10.1016/s0140-6736(05)66418-5 (2005).
Chandramohan, D. et al. Cluster randomised trial of intermittent preventive remedy for malaria in infants in space of excessive, seasonal transmission in Ghana. BMJ (Medical Res. ed.). 331, 727–733. https://doi.org/10.1136/bmj.331.7519.727 (2005).
Penny, M. A. et al. Public well being impression and cost-effectiveness of the RTS,S/AS01 malaria vaccine: a scientific comparability of predictions from 4 mathematical fashions. Lancet 387, 367–375. https://doi.org/10.1016/s0140-6736(15)00725-4 (2016).
Águas, R., Lourenço, J. M. L., Gomes, M. G. M. & White, L. J. The impression of IPTi and IPTc interventions on malaria scientific Burden – In Silico views. PLOS ONE. 4, e6627. https://doi.org/10.1371/journal.pone.0006627 (2009).
World Well being Group. WHO malaria terminology 2021 replace. Report No. WHO/HTM/GMP/2016.6, (Geneva: World Well being Group. (2021). https://apps.who.int/iris/deal with/10665/349442.
Omondi, C. J. et al. Perennial transmission of malaria within the low altitude areas of Baringo County, Kenya. Malar. J. 16, 257. https://doi.org/10.1186/s12936-017-1904-y (2017).
Ashley, E. A. & Yeka, A. Seasonal malaria chemoprevention: closing the know-do hole. Lancet 396, 1778–1779. https://doi.org/10.1016/s0140-6736(20)32525-3 (2020).
Plowe, C. V. Malaria chemoprevention and drug resistance: a overview of the literature and coverage implications. Malar. J. 21, 104. https://doi.org/10.1186/s12936-022-04115-8 (2022).
Steinhardt Laura. Abstract of intermittent preventive remedy in infants (IPTi) contextual components. Part 4.2.2 Perennial malaria chemoprevention (PMC). In WHO Tips for malaria, 3 June 2022. (2022).
Macete, E. et al. Intermittent preventive remedy for malaria management administered on the time of routine vaccinations in Mozambican infants: a randomized, placebo-controlled trial. J. Infect. Dis. 194, 276–285. https://doi.org/10.1086/505431 (2006).
Burgert, L., Reiker, T., Golumbeanu, M., Möhrle, J. J. & Penny, M. A. Mannequin-informed goal product profiles of long-acting-injectables to be used as seasonal malaria prevention. PLOS Glob Public. Well being. 2, e0000211. https://doi.org/10.1371/journal.pgph.0000211 (2022).
Masserey, T., Lee, T., Kelly, S. L., Hastings, I. M. & Penny, M. A. Seasonal malaria chemoprevention and the unfold of Plasmodium falciparum quintuple mutant parasites immune to sulfadoxine-pyrimethamine: a modelling examine. Lancet Microbe. 5, 100892. https://doi.org/10.1016/S2666-5247(24)00115-0 (2024).
Mahaman Moustapha, L. et al. Proof that seasonal malaria chemoprevention with SPAQ influences blood and pre-erythrocytic stage antibody responses of Plasmodium falciparum infections in Niger. Malar. J. 20, 1. https://doi.org/10.1186/s12936-020-03550-9 (2021).
Gosling, R. D., Carneiro, I. & Chandramohan, D. Intermittent preventive remedy of malaria in infants: how does it work and the place will it work? Trop. Med. Int. Well being. 14, 1003–1010. https://doi.org/10.1111/j.1365-3156.2009.02303.x (2009).
de Kock, M. et al. Inhabitants Pharmacokinetic properties of sulfadoxine and pyrimethamine: a pooled evaluation to tell optimum dosing in African youngsters with uncomplicated malaria. Antimicrob. Brokers Chemother. 62, e01370-17. https://doi.org/10.1128/aac.01370-17 (2018).
Masserey, T. et al. The affect of organic, epidemiological, and remedy components on the institution and unfold of drug-resistant plasmodium falciparum. eLife 11, e77634. https://doi.org/10.7554/eLife.77634 (2022).
Delves, M. et al. The actions of present antimalarial medicine on the life cycle phases of plasmodium: a comparative examine with human and rodent parasites. PLoS Med. 9, e1001169. https://doi.org/10.1371/journal.pmed.1001169 (2012).
Masserey, T., Braunack-Mayer, L., Miller, R. S., Möhrle, J. J. & Penny, M. A. A roadmap for Understanding sulfadoxine-pyrimethamine in malaria chemoprevention. Parasitology, Revealed on-line 2025:1–10. https://doi.org/10.1017/S0031182025000071 (2025).
Cairns, M. et al. Length of safety towards malaria and anaemia supplied by intermittent preventive remedy in infants in Navrongo, Ghana. PloS One. 3, e2227–e2227. https://doi.org/10.1371/journal.pone.0002227 (2008).
Kelly, S. L., Malinga, J. & Penny, M. A. Evaluating modelled impression and cost-effectiveness estimates for the RTS,S/AS01 malaria vaccine with analysis outcomes noticed in phased pilot introductions. (2024). https://cdn.who.int/media/docs/default-source/immunization/sage/vpp-background-documents/malaria/path_final-report-on-vaccine-impact-and-cost-effectiveness-estimates6d0e5362-c947-4ff8-b0d5-1c485c0ed8ce.pdf?sfvrsn=371c20a_1.
Gunda, R. & Chimbari, M. J. Value-effectiveness evaluation of malaria interventions utilizing incapacity adjusted life years: a scientific overview. Value Eff. Resour. Alloc. 15, 10. https://doi.org/10.1186/s12962-017-0072-9 (2017).
Conteh, L. et al. Prices and cost-effectiveness of malaria management interventions: a scientific literature overview. Worth Well being. 24, 1213–1222. https://doi.org/10.1016/j.jval.2021.01.013 (2021).
Braunack-Mayer, L. et al. Design and collection of drug properties to extend the general public well being impression of next-generation seasonal malaria chemoprevention: a modelling examine. Lancet Glob Well being. 12, e478–e490. https://doi.org/10.1016/S2214-109X(23)00550-8 (2024).
White, N. J. Intermittent presumptive remedy for malaria. PLoS Med. 2, e3. https://doi.org/10.1371/journal.pmed.0020003 (2005).
Desai, M. et al. Affect of sulfadoxine-pyrimethamine resistance on effectiveness of intermittent preventive remedy for malaria in being pregnant at clearing infections and stopping low delivery weight. Clin. Infect. Dis. 62, 323–333. https://doi.org/10.1093/cid/civ881 (2016).
Nankabirwa, J. et al. Efficacy, security, and tolerability of three regimens for prevention of malaria: a randomized, placebo-controlled trial in Ugandan schoolchildren. PLoS One. 5, e13438. https://doi.org/10.1371/journal.pone.0013438 (2010).
Lahuerta, M. et al. Analysis of well being system readiness and protection of intermittent preventive remedy of malaria in infants (IPTi) in Kambia district to tell Nationwide scale-up in Sierra Leone. Malar. J. 20, 74–74. https://doi.org/10.1186/s12936-021-03615-3 (2021).
Marseille, E., Larson, B., Kazi, D. S., Kahn, J. G. & Rosen, S. Thresholds for the fee–effectiveness of interventions: various approaches. Bull. World Well being Organ. 93, 118–124. https://doi.org/10.2471/BLT.14.138206 (2014).
Agusto, F. B. & IM, E. L. Optimum management and cost-effective evaluation of malaria/visceral leishmaniasis co-infection. PLoS One. 12, e0171102. https://doi.org/10.1371/journal.pone.0171102 (2017).
Bertram, M. Y. & Edejer, T. T. T. Introduction to the Particular Concern on The World Well being Group Selecting Interventions That Are Value-Efficient (WHO-CHOICE) Replace. IJHPM 10, 670–672 (2021). https://doi.org/10.34172/ijhpm.2021.105
Golumbeanu, M. et al. Leveraging mathematical fashions of illness dynamics and machine studying to enhance growth of novel malaria interventions. Infect. Dis. Poverty. 11, 61. https://doi.org/10.1186/s40249-022-00981-1 (2022).
Reiker, T. et al. Emulator-based bayesian optimization for environment friendly multi-objective calibration of an individual-based mannequin of malaria. Nat. Commun. 12, 7212. https://doi.org/10.1038/s41467-021-27486-z (2021).
Smith, T. et al. Mathematical modeling of the impression of malaria vaccines on the scientific epidemiology and pure historical past of Plasmodium falciparum malaria: overview. Am. J. Trop. Med. Hyg. 75, 1–10. https://doi.org/10.4269/ajtmh.2006.75.2_suppl.0750001 (2006).
Smith, T. et al. Ensemble modeling of the probably public well being impression of a pre-erythrocytic malaria vaccine. PLoS Med. 9, e1001157. https://doi.org/10.1371/journal.pmed.1001157 (2012).
Molineaux, L. et al. Plasmodium falciparum parasitaemia described by a brand new mathematical mannequin. Parasitology 122, 379–391. https://doi.org/10.1017/S0031182001007533 (2001).
Nu Htay, M., Hastings, I., Hodel, E. & Kay, Ok. Effectiveness of intermittent preventive remedy in being pregnant with sulfadoxine-pyrimethamine: an in Silico Pharmacological mannequin. Asian Pac. J. Trop. Med. 13, 366–374. https://doi.org/10.4103/1995-7645.289441 (2020).
Kay, Ok. & Hastings, I. M. Enhancing pharmacokinetic-pharmacodynamic modeling to research anti-infective chemotherapy with utility to the present technology of antimalarial medicine. PLOS Comput. Biol. 9, e1003151. https://doi.org/10.1371/journal.pcbi.1003151 (2013).
Okell, L. C. et al. Contrasting advantages of various artemisinin mixture therapies as first-line malaria remedies utilizing model-based cost-effectiveness evaluation. Nat. Commun. 5, 5606. https://doi.org/10.1038/ncomms6606 (2014).
Wilcox, R. R. in In Introduction To Strong Estimation and Speculation Testing (Fifth Version). 253–350 (eds Wilcox, R. R.) (Tutorial, 2022).
Nhama, A. et al. In vivo efficacy and security of artemether–lumefantrine and amodiaquine–artesunate for uncomplicated plasmodium falciparum malaria in Mozambique, 2018. Malar. J. 20 (390). https://doi.org/10.1186/s12936-021-03922-9 (2021).
Russo, G. & McPake, B. Medication costs in city Mozambique: a public well being and financial examine of pharmaceutical markets and value determinants in low-income settings. Well being Coverage Plan. 25, 70–84. https://doi.org/10.1093/heapol/czp042 (2009).
World Well being Group. Regional Strategic Plan for Immunization 2014–2020. (Regional Workplace for Africa:World Well being Group, (2015). https://iris.who.int/deal with/10665/204373.
Berzosa, P. et al. Comparability of three diagnostic strategies (microscopy, RDT, and PCR) for the detection of malaria parasites in consultant samples from Equatorial Guinea. Malar. J. 17, 333. https://doi.org/10.1186/s12936-018-2481-4 (2018).
Griffin, J. et al. Protecting efficacy of intermittent preventive remedy of malaria in infants (ipti) utilizing sulfadoxine-pyrimethamine and parasite resistance. PLoS ONE. 5 (9). https://doi.org/10.1371/journal.pone.0012618 (2010).
von Seidlein, L. et al. A randomized managed trial of Artemether/benflumetol, a brand new antimalarial and Pyrimethamine/sulfadoxine within the remedy of uncomplicated falciparum malaria in African youngsters. Am. J. Trop. Med. Hyg. 58, 638–644. https://doi.org/10.4269/ajtmh.1998.58.638 (1998).