Some communities are “GP deserts”, the place there are too few GPs to make sure everybody can get the care they want once they want it. These communities are sometimes sicker and poorer than the remainder of Australia, however obtain much less care and face greater charges.
On the 2025 federal election, all events ought to decide to altering that. The following authorities – whether or not Labor or Coalition, majority or minority – ought to set a minimal stage of entry to GP care, and fund native schemes to fill the worst gaps.
Folks in GP deserts miss out on care
About half 1,000,000 Australians stay in GP deserts. These are communities in the underside 5% for GP providers per individual. Most GP deserts are in distant Queensland, Western Australia and the Northern Territory, and a few are in Canberra.
Folks in GP deserts obtain 40% fewer GP providers than the nationwide common. This implies much less of the important check-ups, screening and drugs administration GPs present.
Nurses and Aboriginal well being employees assist plug among the hole, however even then GP deserts aren’t near catching as much as different areas.
And a few folks miss out altogether. Final 12 months, 8% of individuals older than 65 in these areas didn’t see the GP in any respect, in comparison with lower than 1% in the remainder of the nation.

Poorer and sicker locations miss out, 12 months after 12 months
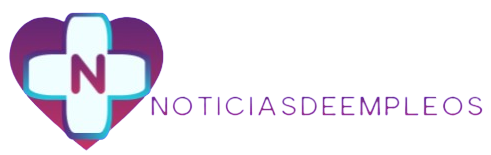
GP deserts are within the worst potential locations. These communities are sometimes sicker and poorer, so they need to be getting extra care than the remainder of Australia, not much less.
Folks in GP deserts are nearly twice extra prone to go to hospital for a situation that may have been prevented with good major care, or to die from an avoidable trigger.
Most GP deserts are within the backside 40% for wealth, but pay extra for care. Sufferers in GP deserts are bulk billed six proportion factors lower than the nationwide common.
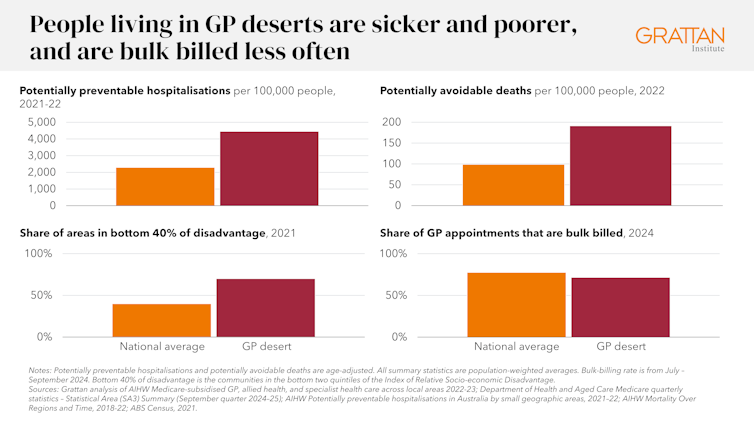
These communities miss out 12 months after 12 months. Whereas rises and falls in nationwide bulk billing charges get headlines, the persistent gaps in GP care are ignored. The identical communities have languished nicely beneath the nationwide common for greater than a decade.
Insurance policies to spice up rural major care don’t go far sufficient
Most GP deserts are rural, so latest insurance policies to spice up rural major care might assist a bit.
In response to rising out-of-pocket prices, the federal government has dedicated A$3.5 billion to triple bulk-billing funds for probably the most deprived. These funds are a lot greater for clinics in rural areas. An uptick in rural bulk billing final 12 months is an early indication it might be working.

Theera Disayarat/Shutterstock
New rural medical faculties and packages ought to assist enhance rural GP provide, since college students who come from, and practice in, rural areas are extra prone to work in them. A “rural generalist” pathway recognises GPs who’ve skilled in an extra ability, resembling obstetrics or psychological well being providers.
However broad-based rural insurance policies should not sufficient. Not all rural areas are GP deserts, and never all GP deserts are rural. Australia additionally wants extra tailor-made approaches.
Native schemes can work
Some communities have taken issues into their very own palms.
In Triabunna on Tasmania’s east coast, a retirement in 2020 noticed residents left with just one GP, forcing folks to journey to different areas for care, typically for nicely over an hour. This was an issue for different cities within the area too, resembling Swansea and Bicheno, in addition to a lot of rural Tasmania.
In desperation, the native council has launched a A$90 medical levy to assist fund new clinics. It’s additionally trialling a new multidisciplinary care strategy, bringing collectively many various well being practitioners to supply care at a single contact level and scale back strain on GPs. Residents get extra care and spend much less effort and time coordinating particular person appointments.
Murrumbidgee in New South Wales has taken a unique strategy. There, trainee medical doctors retain a single employer all through their placements. Meaning they’ll work throughout the area, in clinics funded by the federal authorities and hospitals managed by the state authorities, with out dropping employment advantages. That helps trainees to remain intently linked to their communities and their sufferers. Murrumbidgee’s success has impressed comparable trials in different elements of NSW, South Australia, Queensland and Tasmania.
These are promising approaches, however they put the burden on communities to piece collectively funding to plug holes. With out safe funding, these fixes will stay piecemeal and precarious, and threat a bidding conflict to draw GPs, which would depart poorer communities behind.
Australia ought to assure a minimal stage of GP care
The federal authorities ought to assure a minimal stage of normal apply for all communities. If providers funded by Medicare and different sources keep beneath that stage for years, funding ought to robotically turn into accessible to bridge the hole.
The federal and state governments must be accountable for fixing GP deserts. These areas sometimes have small populations, few clinicians, and restricted infrastructure. So governments should work collectively to make the perfect use of scarce assets.

Stephen Barnes/Shutterstock
Funding should be versatile, as a result of each GP desert is totally different. Generally the answer could also be so simple as serving to an present clinic rent additional employees. Different communities could need to arrange a brand new clinic, or introduce telehealth for routine check-ups. There isn’t a lack of concepts about the right way to shut gaps in care, the issue lies in funding them.
Lifting all GP deserts to the highest of the desert threshold – or guaranteeing no less than 4.5 GP providers per individual per 12 months, adjusted for age, would price the federal authorities no less than A$30 million a 12 months in Medicare funds.
Offering additional providers in GP deserts will likely be dearer than common. However even when the fee was doubled or tripled, it will nonetheless be solely a fraction of the billions of {dollars} of additional incentives GPs are attending to bulk invoice – and it will remodel the communities that need assistance probably the most.
GP deserts didn’t seem in a single day. Successive governments have left some communities with too little major care. The looming federal election offers each celebration the chance to make amends.
In the event that they do, the subsequent time period of presidency might see GP deserts eradicated for good.